Radiation oncology clinics face numerous challenges in the present environment, including the simultaneous management of multiple tasks (many of which are manual in nature), various degrees of standardisation, and the potential for errors to impact patient treatment. Automation can help address these challenges by reducing the time required to execute manual portions of the workflow and positively impacting the quality and safety of patient care. Tyler Blackwell, Medical Physicist discusses more:
Efficiency
To a large degree, many departments have already integrated automation into their departments. However, it stands to be a driving force of innovation in our field for the foreseeable future, coinciding with efforts to improve plan quality and reduce errors inherent in human interaction. Increasing the productivity and efficiency of our daily clinical tasks by minimizing time spent on tedious, routine tasks “below our licenses” (as worded by physicist Eric Ford as part of a Radformation Focal Spot interview) allows more time to address other critical clinical elements that require human expertise.
In developing smarter tools, we have an opportunity to improve the patient experience. Radformation CEO Kurt Sysock, MS, DABR, explains, “On average, it takes five days after simulation to create a finished plan that is ready for treatment, and we want to reduce that to less than one day.” Indeed, reducing the time between simulation and treatment can have a significant impact not only on patient satisfaction, but also on patient outcomes. Delays in treatment planning times are associated with an overall higher risk of mortality ranging from 1.2–3.2% per week for curative diseases. Reducing the time between simulation and treatment maximizes tumor control probability and patient survival.
Quality and Safety
The quality and consistency of patient care are greatly improved when the care team is able to deliver treatment as efficiently as possible. In this environment, they can devote more resources toward tasks that require greater attention or collective experience. From the clinician’s point of view, smart automation reduces the time spent on tasks that do not add value to patient care but are nonetheless important for sustaining operations.
Over the last decade, clinicians have largely embraced a culture of safety and quality improvement. This paradigm shift delivers a number of benefits for patients and involves a continued effort toward reducing errors in radiation oncology. While a number of interventions can positively influence safety and quality, automation is highly effective in this regard. Absent automation, this ongoing commitment will be inhibited by a lack of efficiency and scalability as clinicians grapple with manual processes and endless checklists.
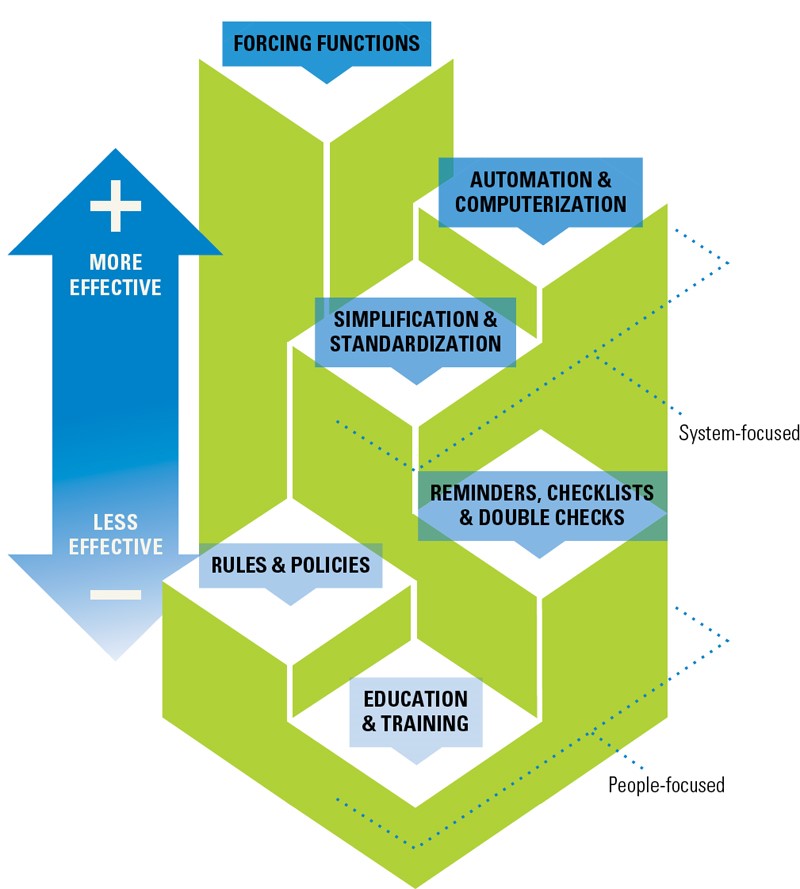
Automation is one of the most effective ways to impact change in medicine. Source: Cafazzo, J and St-Cry, O. From Discovery to Design: The Evolution of Human Factors in HealthCare. Healthcare Quarterly. April 2012. doi:10.12927/hcq.2012.22845
Automation plays a part in advances in clinical care as well. Radformation CSO Alan Nelson, DMP, DABR, argues that, “just as IMRT significantly improved the effectiveness of treatment while reducing side-effects, automation will enable the field to explore and implement new solutions for therapy protocols that otherwise simply would not have been feasible due to lack of resources.”
An Elevated Workflow At Every Step
Finding steps along the treatment care path that involve manual inputs isn’t a challenge. Wherever they exist, there is an opportunity for automation to provide value. From planning and on-treatment to billing and quality assurance, the results of these workflow improvements are impressive.
Structure Segmentation
The proper delineation of anatomical structures in the vicinity of the target is important in understanding the impact of a treatment plan on the surrounding healthy tissues. But manual contouring can be resource-intensive, and some structure boundaries—especially for target structures—can vary widely based on who is performing the work. According to physicist Noah Bice of New York University Langone, “Contouring is subjective. With any mix of individuals, there are inherently varying levels of expertise and personal preference involved.”
Within the past few years, the introduction of deep-learning algorithms for contouring has transformed the landscape. By exploiting cloud-based computational resources, structure sets, including organs-at-risk and target structures, can be generated in a fraction of the time as manual contours. Departments have been quick to adopt this new technology, which will likely become a global standard of care within the decade.
Treatment Planning
Given that every patient’s anatomy and disease state is unique, it might feel safe to assume that it may not be possible to automate this process. Despite this inherent variation, the approach to planning is algorithmic and repetitive. By scripting various repetitive processes—field-in-field or electronic compensator planning, for example—departments are capable of producing consistently high-performing plans in a fraction of the time.
This process, when applied to the Halcyon machine, has made it feasible to plan electronic compensator breast plans when otherwise manual planning is impractically cumbersome and time-consuming.
Plan Evaluation and Reporting
Determining the quality of any given treatment plan is no small task. Often, it is not easy to compare comprehensive plan quality elements within the treatment planning system (TPS). By tapping into the plan data via scripting interfaces, it’s possible to pull dosimetric information for comparison against dose constraint templates to verify the quality of a plan during or after the plan is complete.
Automated platforms are quickly becoming the standard of care, providing intuitive assessments of plan quality, including dose constraints, plan checks, machine collision risk, and reporting. While default TPS reports are often limited in scope, third-party options offer fast, customized plan reports as well as the ability to populate directly into ARIA Documents.
Comprehensive new tools allow for faster, user-friendly plan revaluation and reporting.
Quality Assurance
Collecting and sorting quality assurance information can be a challenging task given the variety of equipment and vendor products in the clinic that requires tracking. The frequency of the tasks adds another layer of complexity as well, with new data being acquired daily. Thankfully, new quality assurance platforms make short work of managing this data, providing a central location for all data from linacs and CTs to ionisation chambers and GM meters. Automation is capable of detecting new test information—from daily or monthly tests—and effortlessly syncing data to the centralized platform for quick analysis and review. These databases bring efficiency while reducing the dependency on multiple separate spreadsheets in unique locations.
Conclusion
In conclusion, the use of intelligent automation in radiation oncology—such as the solutions offered by Radformation—has the potential to revolutionize clinical workflows, leading to bottom-line improvements in patient care. By reducing the time required to execute manual portions of the workflow, clinicians can devote more time to critical clinical elements that require human expertise, such as addressing treatment planning and ensuring patient safety. Automation also plays a part in advances in clinical care and enables the field to explore and implement new solutions that may not have been feasible without this technology. In short, the benefits of automation in radiation oncology are numerous and diverse, and they can significantly enhance the overall quality and safety of patient care.
To learn more about how automation can play a role in your department, visit us at Radformation’s booth at BIR’s Annual Radiotherapy an Oncology Meeting 2023 where we will highlight our workflow automation solutions. See the possibilities for improving clinic efficiency and effectiveness with products, including AutoContour for autosegmentation and RadMachine for machine QA, by scheduling a demonstration today.
About Tyler Blackwell
Tyler Blackwell, MS, DABR, is a medical physicist at Radformation focused on clinical collaborations and community engagement. Before joining Radformation, he spent a decade working as a clinical physicist. He is active on several committees for the American Association of Physicists in Medicine, including the board of directors, and volunteers for the American Board of Radiology.

